Simplify Approvals with a Previous Permission Online Aide

2025-06-27 03:53
11
0
본문
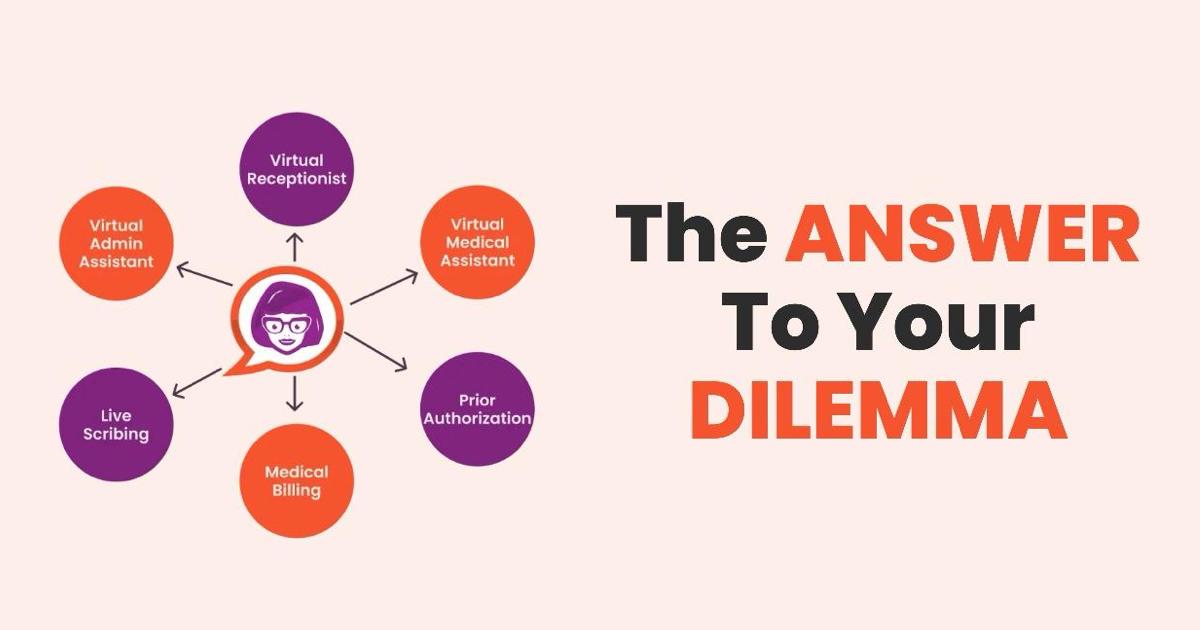
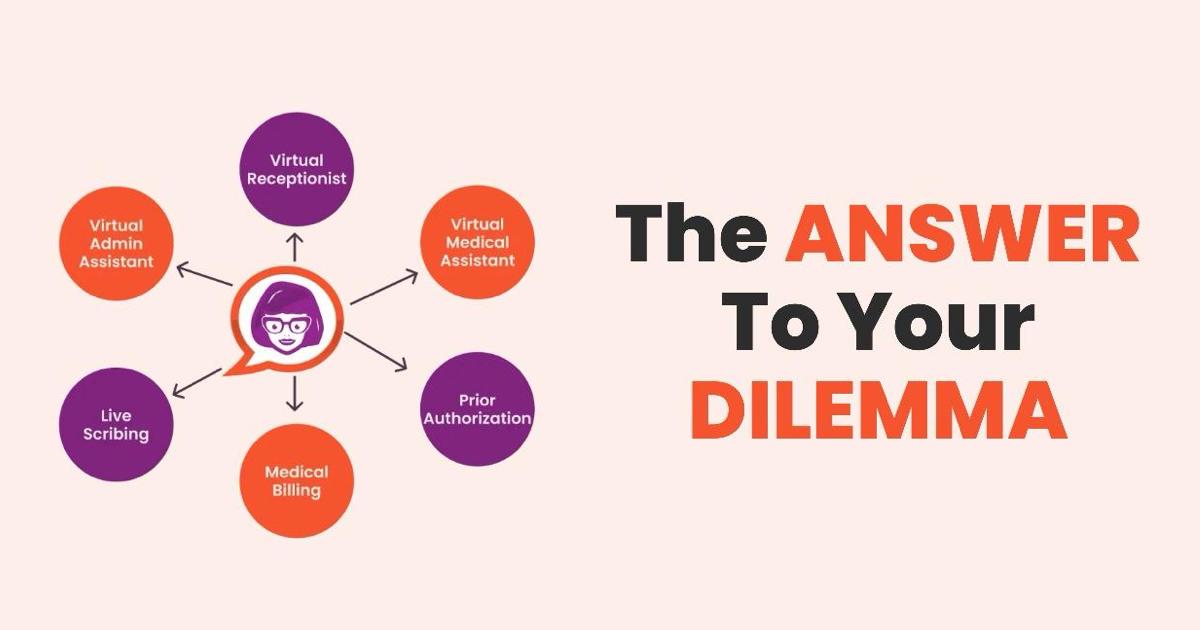
In today's busy healthcare setting, prior authorization can be a traffic jam that delays care, worries personnel, and discourages clients. A Prior Consent Virtual Assistant ( VA) modifications that-- simplifying authorizations and accelerating client accessibility to required therapies.
What Is a Previous Authorization Digital Aide?
A Previous Permission Virtual Assistant is a skilled remote professional that takes care of and sends prior consent demands on part of healthcare companies. These VAs are experienced in insurance confirmation, clinical coding, payer-specific standards, and follow-up communication with insurance companies. They function effortlessly with your EHR and invoicing systems to soothe your internal group of the lengthy approval procedure.
Why Prior Authorizations Reason Center Mayhem
According to the American Medical Association (AMA), doctors and their personnel full nearly 45 previous consent requests weekly, with each one taking around 14 hours of team time. That's virtually two complete days lost-- weekly.
The consequences include:
Delayed patient treatment
Burnout amongst clinical team
Denied claims and earnings loss
Decreased individual contentment
Just How a Virtual Aide Simplifies the Refine
A Prior Authorization VA takes the weight off your clinic's shoulders with these essential benefits:
✅ 1. Faster Turn-around Times
Digital assistants concentrate on previous auth workflows, enabling them to submit tidy, full demands that minimize back-and-forth with insurer.
✅ 2. 24-- two days Handling
Many VAs work across time areas, which implies your clinic can continue refining requests outside traditional hours, quickening authorizations for immediate instances.
✅ 3. Fewer Mistakes and Denials
VAs make certain the right ICD-10 and CPT codes are made use of which medical need is plainly recorded, resulting in less denials and charms.
✅ 4. EMR Integration
They work within your clinic's systems-- like Athenahealth, Legendary, eClinicalWorks, or NextGen-- so there's no requirement to re-train your personnel or migrate platforms.
✅ 5. Cost-Effective Staffing
Employing a VA is significantly much more inexpensive than onboarding a permanent internal organizer. And also, you save on training, advantages, and office expenses.
What to Look for in a Prior Authorization VA
. Not all virtual assistants are produced equal. Try to find:.
Medical workplace or payment experience.
Experience with your state's Medicaid and top personal payers.
Understanding of clinical terminology and medical paperwork.
Strong interaction abilities for carrier and payer communications.
HIPAA-compliant procedures and safe remote systems.
Real-World Outcomes.
Clinics making use of Previous Consent VAs record:.
40-- 60% faster approvals.
30% fewer insurance coverage denials.
Approximately 50% staff time saved on admin tasks.
Greater client complete satisfaction scores.
Final Thoughts: Allow Your Staff Focus on Individual Care.
If your facility is battling with taxing prior auth procedures, docva.com it's time to delegate to a Previous Permission Digital Aide. These experienced experts handle the backend turmoil so your group can concentrate on what truly matters-- delivering top quality care to your clients.
A Prior Authorization Virtual Aide is a qualified remote professional who handles and sends prior consent requests on behalf of medical care service providers. These VAs are experienced in insurance coverage confirmation, clinical coding, payer-specific standards, and follow-up communication with insurance companies. They function flawlessly with your EHR and invoicing systems to alleviate your internal group of the taxing approval process.
 What to Look for in a Previous Consent VA
What to Look for in a Previous Consent VA
. Not all online aides are created equal.
What Is a Previous Authorization Digital Aide?
A Previous Permission Virtual Assistant is a skilled remote professional that takes care of and sends prior consent demands on part of healthcare companies. These VAs are experienced in insurance confirmation, clinical coding, payer-specific standards, and follow-up communication with insurance companies. They function effortlessly with your EHR and invoicing systems to soothe your internal group of the lengthy approval procedure.
Why Prior Authorizations Reason Center Mayhem
According to the American Medical Association (AMA), doctors and their personnel full nearly 45 previous consent requests weekly, with each one taking around 14 hours of team time. That's virtually two complete days lost-- weekly.
The consequences include:
Delayed patient treatment
Burnout amongst clinical team
Denied claims and earnings loss
Decreased individual contentment
Just How a Virtual Aide Simplifies the Refine
A Prior Authorization VA takes the weight off your clinic's shoulders with these essential benefits:
✅ 1. Faster Turn-around Times
Digital assistants concentrate on previous auth workflows, enabling them to submit tidy, full demands that minimize back-and-forth with insurer.
✅ 2. 24-- two days Handling
Many VAs work across time areas, which implies your clinic can continue refining requests outside traditional hours, quickening authorizations for immediate instances.
✅ 3. Fewer Mistakes and Denials
VAs make certain the right ICD-10 and CPT codes are made use of which medical need is plainly recorded, resulting in less denials and charms.
✅ 4. EMR Integration
They work within your clinic's systems-- like Athenahealth, Legendary, eClinicalWorks, or NextGen-- so there's no requirement to re-train your personnel or migrate platforms.
✅ 5. Cost-Effective Staffing
Employing a VA is significantly much more inexpensive than onboarding a permanent internal organizer. And also, you save on training, advantages, and office expenses.
What to Look for in a Prior Authorization VA
. Not all virtual assistants are produced equal. Try to find:.
Medical workplace or payment experience.
Experience with your state's Medicaid and top personal payers.
Understanding of clinical terminology and medical paperwork.
Strong interaction abilities for carrier and payer communications.
HIPAA-compliant procedures and safe remote systems.
Real-World Outcomes.
Clinics making use of Previous Consent VAs record:.
40-- 60% faster approvals.
30% fewer insurance coverage denials.
Approximately 50% staff time saved on admin tasks.
Greater client complete satisfaction scores.
Final Thoughts: Allow Your Staff Focus on Individual Care.
If your facility is battling with taxing prior auth procedures, docva.com it's time to delegate to a Previous Permission Digital Aide. These experienced experts handle the backend turmoil so your group can concentrate on what truly matters-- delivering top quality care to your clients.
A Prior Authorization Virtual Aide is a qualified remote professional who handles and sends prior consent requests on behalf of medical care service providers. These VAs are experienced in insurance coverage confirmation, clinical coding, payer-specific standards, and follow-up communication with insurance companies. They function flawlessly with your EHR and invoicing systems to alleviate your internal group of the taxing approval process.
 What to Look for in a Previous Consent VA
What to Look for in a Previous Consent VA. Not all online aides are created equal.

댓글목록0
댓글 포인트 안내